Local healthcare providers preparing for COVID-19
Published 8:06 pm Friday, March 20, 2020
|
Getting your Trinity Audio player ready...
|
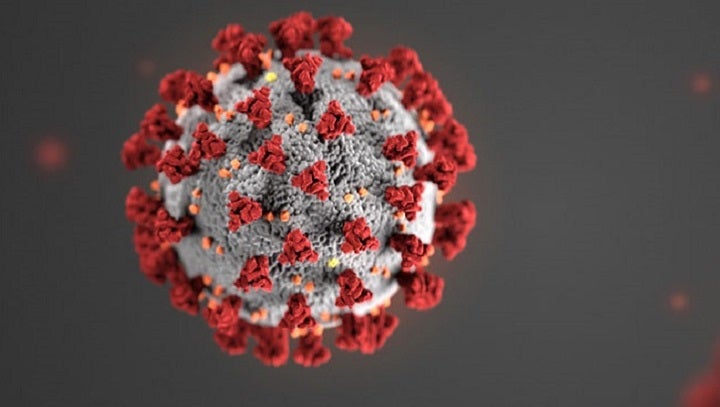
There are now 106 confirmed cases of COVID-19 Coronavirus in Alabama, and although none are in Pike County, local healthcare providers are preparing for local cases.
Rick Smith, CEO at Troy Regional Medical Center, said about 40 local patients have been tested, and all that have been returned have come back negative.
The hospital is taking extra precautions to prevent the spread of the disease to any other patients or employees.
“Here at the hospital, we’re careful not to overload elevators and we use stairwells when possible,” Smith said. “We have had to block access to the cafeteria to the public, which is unfortunate because the community has enjoyed that over the years. Our team members are going to do whatever it takes to take care of patient. Limiting the number of visitors in the building is the most key aspect of this to avoid unnecessary exposure.”
The hospital had already cut back visitation drastically before the Alabama Department of Public Health ordered to cease all visitations outside of end-of-life and maternity situations.
Smith said the process has been running smoothly so far and urged residents to continue to follow CDC and ADPH guidance, including what to do if one suspects he or she or a family member has contracted the virus.
“If you feel like you have symptoms, contact your primary healthcare provider,” Smith said. “They may test you for strep and flu there. After their screening, they’ll send you here. We’ll collect the specimen and then we will send it to either the state lab or one of the private labs for testing. It all starts with that conversation with your primary care provider.”
Ivy Creek Family Care of Troy is another one of the local places collecting specimens, along with SARHA.
Allison Lecroy McCullough, assistant office manager, further explained the process.
“We are meeting everyone outside and checking for temperatures more than 100.4,” McCullough said. “We are doing tele-visits with primary care patients so that they don’t have to come into the office.”
According to the CDC, clinicians should use their judgment to determine if a patient has signs and symptoms compatible with COVID-19 and whether the patient should be tested. Most patients with confirmed COVID-19 have developed fever and/or symptoms of acute respiratory illness (e.g., cough, difficulty breathing).
With a backlog of tests and a shortage of supplies, the CDC also offers guidelines for prioritizing testing:
• Hospitalized patients who have signs and symptoms compatible with COVID-19 in order to inform decisions related to infection control.
• Other symptomatic individuals such as, older adults and individuals with chronic medical conditions and/or an immunocompromised state that may put them at higher risk for poor outcomes (e.g., diabetes, heart disease, receiving immunosuppressive medications, chronic lung disease, chronic kidney disease).
• Any persons including healthcare personnel2, who within 14 days of symptom onset had close contact3 with a suspect or laboratory-confirmed4 COVID-19 patient, or who have a history of travel from affected geographic areas5 (see below) within 14 days of their symptom onset.
If testing will be conducted through ADPH, the healthcare provider takes a nasopharyngeal (swab from the nose), using the same kind of swab used for flu tests. The specimen is then put in a viral transport media – again, the same thing used to transport specimens being tested for flu and other viruses. The specimen is shipped overnight to the State Lab, where a COVID-19 test kit provided by the CDC is used to check for the virus.
One of the concerns as the diseases spreads is the strain it will put on hospitals.
Smith said there is an online portal that ensures all Alabama hospitals can access resources statewide to determine where demand is needed.
“The Alabama Instant Management System (AIMS) is a clearinghouse if you will of all the hospitals to input our data,” Smith said. “It tracks available beds, ICU beds, ventilators – too many things to name. I think that the largest concern is our access to the most critical supplies like personal protective equipment (PPE) – the gowns and masks and eye shields and things of that nature. We’ve made a request through this AIMS system and been ensured additional supplies are on the way – but of course everybody is using that and some manufacturers overseas are somewhat limited. That’s the most challenging aspect of what we’re doing right now.”
The key now, Smith said, is for residents to continue following the CDC and ADPH protocols of social distancing and avoiding large gatherings to prevent the spread of the coronavirus to keep hospitals and healthcare providers from becoming strained and overcrowded. The guidance asks residents to keep six feet of distance form others and to wash and sanitize hands regularly.
By staying at home and avoiding others as much as possible, medical professionals hope to “flatten the curve” of the disease, or reduce the drastic increase of the spread to better manage patients.